Covid-19 is so much in the news, and in public statements by the member for the Hughes electorate, that it seems helpful for us all to understand viruses and vaccinations.
I’m not a medical professional, so I have prepared this summary of the information available from medical professionals and authoritative medical organisations. I’m hoping you may find this summary as informative as I have.
Understanding DNA
To understand viruses and vaccines, we need to have a very basic understanding of DNA.
DNA (Deoxyribonucleic Acid) is a complex organic molecule that stores enormous amounts of information which controls how our body grows, by providing code to make the different protein molecules which make up different parts of the body.
DNA molecules are made up of two strands which curl around each other in the famous “double helix” shape. Along each strand are nucleotides (a sugar based molecule), each of which links with a nucleotide on the other strand, so the structure is akin to a coiled ladder, with each rung made up of a nucleotide pair. There are four types of nucleotides, labelled A, C, G and T after their chemical names, and are sometimes called DNA bases. The human genome has almost three billion bases.

The nucleotides in DNA form a code that contains the instructions needed for an organism to develop, survive and reproduce. To carry out these functions, DNA sequences must be converted into messages that can be used to produce proteins, which are the complex molecules that do most of the work in our bodies.
RNA (Ribonucleic acid) is a molecule similar to DNA that has many roles in cellular processes, including converting the information stored in DNA into proteins.
What are viruses?
Viruses are tiny (microscopic) infectious agents that grow and multiply only inside living cells of an organism.
A virus is not considered to be a living organism (it can’t capture or store energy for itself or survive for long independent of a host), but rather a biochemical mechanism (a “molecular machine”). Viruses are the most common biological entities on Earth and the smallest type of parasite known.
The core of a virus particle (or “virion”) is a DNA or RNA molecule that contains the genetic instructions for reproducing the virus. This is wrapped up in a coat made of protein molecules which protects the genetic material and enables it to exist outside a host cell for a period of time. Eventually they either break down and “die” or come into contact with a cell that can become a host.
Washing with soap breaks down the protective outer coating of the coronavirus, thus destroying its ability to infect, making hand-washing an important preventative.
Viruses rely on the cells of other organisms to survive and reproduce. A virion attaches to a suitable host cell and penetrates the cell. Once inside, the virus “hacks” the cell and uses the cell’s reproductive processes to produce more viruses, which move out of the cell and infect more cells. This process often destroys the cell.
Viruses are among the most destructive of parasites, causing diseases such as Mumps, Measles, Polio, Smallpox, Chickenpox, Flu (influenza), HIV/AIDS, Ebola and Covid-19. Viruses can also infect plants and animals.
Viruses can evolve into new forms rapidly. Some new forms will be less effective and will not multiply, but occasionally a new variant is more contagious and it will quickly become the dominant strain as it out-competes the earlier strains. For this reason, the longer a virus remains active in the community, because vaccination rates are too low, the more likely more harmful forms will evolve.
The human immune system
The human immune system has evolved to fight off pathogens such as bacteria, viruses, parasites or fungi that can cause disease within the body. When a pathogen invades the body, the immune system produces antibodies that recognise and fight one specific molecule on the outside of the pathogen, called an antigen.
When the human body is exposed to an antigen for the first time, it takes time for the immune system to respond and produce antibodies specific to that antigen. But once created, the body retains the ability to quickly produce the antibodies if invaded again by the same pathogen. As a result, there are thousands of different antibodies in our bodies.
In many cases the human immune system is capable of fighting off the virus, but in some cases it cannot easily do so without assistance.

Vaccines
Vaccines assist the body to respond to pathogens by preparing the immune system in advance so that it already has the ability to make antibodies quickly when attacked. They have been instrumental in eliminating Smallpox and in effectively treating Polio, Tetanus, Flu, Hepatitis, Rubella, Measles, Mumps, Chickenpox and many more diseases.
Vaccines worked by teaching our immune system how to cope with a threat. They introduce a harmless substance into the body and the immune system reacts by producing antibodies. Then when the real virus appears, the body is ready.
Most vaccines use a harmless part of a virus, a dead virus, a harmless form of a virus, or an inert version of a toxin to provoke the immune system.
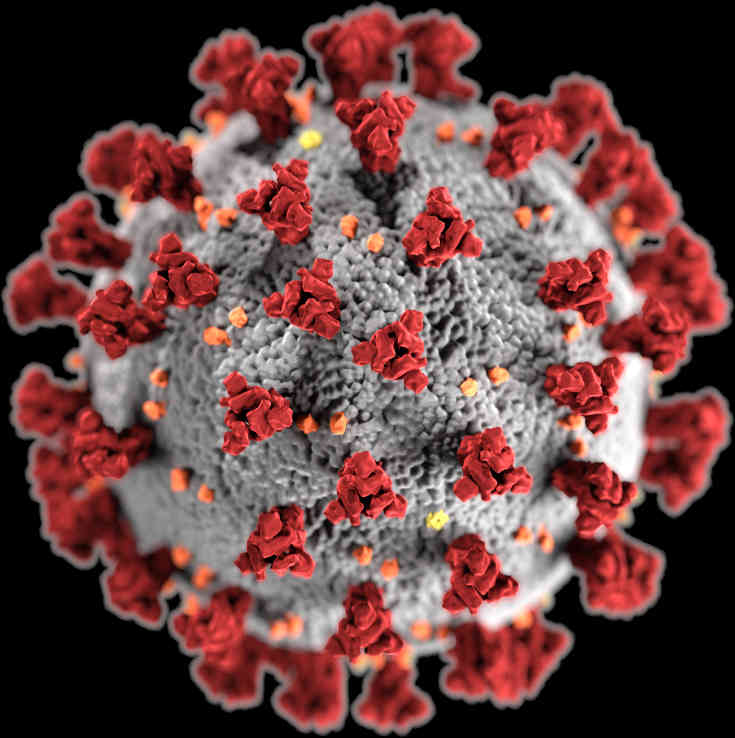
At least one Covid-19 vaccine in development works this way, by injecting a small part of the virion, the spike protein. (The spike proteins, shown in red in the graphic at the top, assist the coronavirus to bind to the surface of a cell.) However this process is slow because it takes time to grow the large amounts of viruses required.
The vaccines available or soon to be available in Australia use a different approach. Instead of injecting part of the coronavirus, they contain instructions obtained from the genetic sequence of the spike protein and inject this genetic code. The body then produces harmless spike proteins, the immune system builds antibodies, and the body is prepared for the real thing.
The Pfizer and Moderna vaccines use synthesised mRNA (messenger RNA) to create spike protein in the body. The AstraZeneca vaccine puts the required DNA to produce the spike protein in the body into a harmless virus which is injected.
Both types teach the body’s immune system how to respond. Both could be developed far quicker than the more conventional vaccines, but both have some drawbacks. Moderna and Pfizer require careful storage and transport to avoid breaking down the delicate mRNA, while the body can build resistance to the AZ vaccine over time.
Antivirals and Covid
There has been much talk about the possible use of antivirals such as hydroxychloroquine, ivermectin and remdesivir for Covid-19 treatment.
Antiviral medicines generally target specific viruses. They work differently depending on the drug and virus type. Antivirals can:
- Block receptors so viruses can’t bind to and enter healthy cells.
- Boost the immune system, helping it fight off a viral infection.
- Lower the viral load (amount of active virus) in the body by attacking the virus directly.
If possible, antivirals should target particular proteins which they disable. These proteins should be as unlike human proteins as possible, to avoid side effects.
Antivirals are an obvious way to try to fight Covid. In an effort to come up with an effective treatment quickly, researchers have tested existing antivirals to see if any are effective against Covid-19. They have generally have been found to show some promise in initial studies, but insufficient benefit in controlled trials to justify use, especially since they have known side effects.
Trials continue, and some reports indicate that new antivirals may become available that will specifically target coronavirus.
Hydroxychloroquine and ivermectin
These two antivirals have been much touted as alternative treatments for Covid-19, but they are not recommend for use in Australia.
- Hydroxychloroquine is a common treatment for malaria and certain autoimmune diseases. Studies indicate that it has no discernible benefit in reducing hospitalisation or death, but it may be useful to reduce the symptoms of mild cases. It can have serious side effects, and may interfere with the body’s immune response to the coronavirus.
- Ivermectin is design as an antivirus – it targets parasites (e.g. head lice, scabies) but it may have antiviral properties. It is often used on animals but also humans (the two forms are different). It has some promise in inhibiting Covid-19, but again significant side effects and possible interference with other medications make it risky.
- Remdesivir is a broad spectrum antiviral that has been used to treat Ebola, but it may cause liver damage. It may be more useful than the previous two drugs for treating Covid-19.
Medical experts in Australia and most developed countries don’t recommend the use of these antivirals. They have concluded that careful behaviour (masks, hand-washing, social distancing, etc) plus a quick rollout of vaccines, is a safer and more effective approach.
Conclusion
Getting vaccinated as soon as possible will not only help each of us resist Covid-19 if we come into contact with it, but will help reduce the viral load in the community. Those who can’t, or won’t, get vaccinated are a danger to others, and depend on the rest of us to reduce the risks they face.
In the long term, specially purposed antivirals may prove more useful than vaccines against Covid-19, but at present vaccination is the most effective protection. Re-purposed antivirals put more dangerous biochemicals into the body than does vaccination. Promoting popular re-purposed antivirals can be dangerous and is irresponsible.
References
- Deoxyribonucleic Acid (DNA) Fact Sheet. National Human Genome Research Institute.
- RNA Functions. Scitable.
- What is a virus? News Medical.
- What is a virus? How do they spread? How do they make us sick? The Conversation.
- How do vaccines work? World Health Organisation.
- Vaccine Preventable Diseases. Australian Government Department of Health.
- Diseases You Almost Forgot About (Thanks to Vaccines). US Centers for Disease Control and Prevention.
- How do COVID-19 vaccines work? Australian Government Department of Health.
- Understanding mRNA COVID-19 Vaccines. US Centers for Disease Control and Prevention.
- mRNA vaccines, explained. Vox on Youtube.
- Antivirals. Cleveland Clinic.
- Antiviral drug: Vaccinations. Wikipedia.
- From hydroxychloroquine to ivermectin: what are the anti-viral properties of anti-parasitic drugs to combat SARS-CoV-2? Oxford Academic Journal of Travel medicine, January 2021.
- Coronavirus disease (COVID-19) advice for the public: Mythbusters. World Health Organisation.
- Antiviral medicines and the treatment of COVID-19. NPS Medicinewise.
- Beyond Anti-viral Effects of Chloroquine/Hydroxychloroquine. Vincent Gies et al, Frontiers in Immunology, July 2020.
- Why You Should Not Use Ivermectin to Treat or Prevent COVID-19. US Food and Drug Administration.
Main graphic: SARS-CoV-2 created at the Centers for Disease Control and Prevention (CDC) by Alissa Eckert, MS; Dan Higgins, MAM, and in the Public Health Image Library of the CDC. The name “coronavirus” comes from the spikes that adorn the outer surface of the virus, which impart the look of a corona surrounding the virion, when viewed electron microscopically.
DNA diagram by US National Library of Medicine.
Vaccination photo by Gustavo Fring from Pexels